How Can the Patient Journey in Oncology be Improved?

DATE
June 07, 2022
AUTHOR
Sascha | Co-Founder & CEO
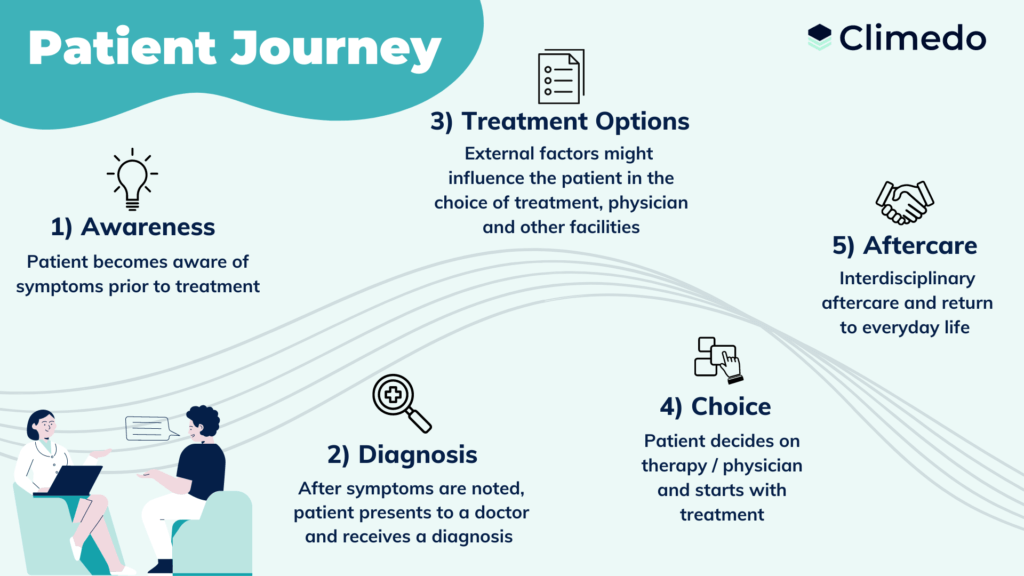
The International Agency for Research on Cancer estimates the number of new cancer cases around 19.3 million worldwide for 2020. This number is expected to increase to around 30 million cases by 2040. With cancer, patients go through similar stages of the patient journey, depending on the grade and type of cancer. Often in oncology, these steps include:
- Recognition of symptoms
- Making an accurate diagnosis
- Selection of appropriate therapies
- Treatment with repeated cycles
- Cure, aftercare or pain relief
The better the data basis, which can be determined, for example, as part of the patient journey, the more efficiently treatment and research can achieve progress. This is why digital tools are on the rise to improve communication between all stakeholders and to involve patients more in the entire treatment process.
However, according to a recent study, Germany ranks second to last out of 17 countries in terms of digital development in the health sector. Therefore exists a need to catch up regarding awareness of the potential that digital solutions can unleash in the context of cancer research. In addition, many patients complain about typical challenges such as the lack of individualized information, poor integration into the entire patient journey and a high administrative burden.
We will show you how to improve the chances of treatment and patient retention in oncology studies with an optimized patient journey and digital tools.
What is it about?
1) Precise classification of symptoms on time
2) Diagnosis with patient focus
3) Tailor the choice of therapy individually to the patient
4) Actively involve cancer patients in the treatment phase
5) Improve aftercare through interdisciplinary services
1) Precise classification of symptoms on time
Awareness of cancer is of great importance for the early detection of tumors. Many patients are not always able to accurately identify the first symptoms and therefore consult a specialist for general medicine. To save valuable time, broader awareness among both doctors and patients can be promoted through comprehensive information, counseling and education campaigns. These services can be provided in a decentralized way through the use of digital technologies and individual video consultations. To diagnose cell changes, which are difficult to detect, medical staff in oncology also need to know about the latest screening methods.
2) Diagnosis with patient focus
After referral, the oncologist carries out the in-depth diagnosis – a phase of great uncertainty for the patient. If the information given to the patients is incomplete or even incorrect and wrong findings are made, this can not only result in expensive, unsuitable treatments, but also cause a lot of unnecessary stress for cancer patients. Therefore, the diagnosis process needs to become much more patient focused.A close exchange between patients, specialists and general practitioners is essential. E-health tools such as digital consultation rooms can already ensure that all parties receive the relevant information quickly. By offering personalized information before and after diagnosis, fears can be reduced. As a result, patients are more willing to accept the treatment and deal with the stressful time mentally strengthened. In addition, this is a way to avoid misinformation that patients get from doing their own research without expert advice.
3) Tailor the choice of therapy individually to the patient
Types of cancer are as varied as patients themselves. Therefore, when choosing a suitable oncology treatment plan, it is important to consider which therapy is particularly promising in each individual case. Within the framework of in-depth counseling services, you can support patients in finding a suitable therapy center, for example. Proximity to the place of residence or the availability of clinical studies are important factors that have a positive effect on the participation of the patients and thus on the chances of success of the therapy.
In addition, medical staff should have sufficient and the latest knowledge in terms of the causes of cancer so that a tailored therapy can be chosen. This can increase the success of the therapy and additionally create confidence in the further steps.
Infographic: Digital Patient Journey in Healthcare
Our infographic shows the benefits of an optimized patient journey and how you can outline the ideal patient journey in 5 steps, including: :
- Awareness
- Diagnosis
- Choice of Treatment
- Therapy Cycles
- Follow-up
4) Actively involve cancer patients in the treatment phase
The treatment phase in oncology is characterized by repetitive therapies such as radiation or chemotherapy, which are accompanied by strong side effects. The use of e-health technologies can make an immense contribution to reduce the administrative burden on patients. It can also improve the treatment environment. For example, stress and waiting times in the run-up to treatment appointments can be reduced by asking patients to complete an online check-in via tablet from their living room. All necessary forms can be filled out at home.
Consumer devices and sensors worn on the body can give patients the feeling of being an active part of the treatment. Such wearables, which allow remote monitoring of the patient, lead to increased engagement as well as individual health data over a longer period of time. These insights help to better understand individual cancers and their progression. Optimized data collection and the use of digital tools, especially during the treatment phase in oncology, make it easier to optimize treatment methods and increase the chances of recovery.
5) Improve aftercare through interdisciplinary services
Ideally, the progress of cancer development can be prevented or it can even be completely eliminated. In the worst case scenario, the disease progresses inexorably and tumors develop again. In this final phase of the patient journey, many patients suffer from depression, persistent fatigue and are overwhelmed when trying to find their way back into everyday life. Interdisciplinary support services such as psychological support or supervised discussion groups with cured patients are an important support here. The use of digital communication tools such as chat rooms or video counseling can also help to overcome barriers in this phase and provide valuable insights.
The way back into everyday life is facilitated by app based offers for planning the day. For example, reminders to take medication, diet adjustments or diary functions can be set. Not only the patients benefit from this: the collected data helps doctors in charge to better document the post-treatment phase and gives research additional clues, for example to be able to further develop cancer drugs.
Conclusion: An optimized, digitally supported patient journey improves oncology care
Many patients feel alone during the oncology patient journey due to poor engagement and insufficient information sharing, causing them to lose confidence in treatment. The use of digital technologies in cancer can chang this: in all phases of medical care, from prevention to follow-up, corresponding e-health tools contribute to optimizing the knowledge of doctors, researchers and patients. Requirements therefore are, for example, consistent data and communication standards as well as the increased use of health data.
Would you like to focus on patient orientation and use digital tools for your next clinical study in oncology? Feel free to reach out to us or schedule a software demo! We look forward to supporting you in the digitalization of your clinical data capture.






